For Adults 55+ Who Want to Feel Steady in Everyday Movement
Balance Confidence Starts with Understanding — Not Guesswork
A simple system designed by a Doctor of Physical Therapy to help you feel steady on stairs, curbs, and daily movements — in just 10 minutes a day, at home.

Something Often Begins to Change After 55
Not suddenly. Not dramatically. Just gradually.
Standing up takes a bit more thought. Turning feels slightly less automatic. Stepping off a curb brings a brief pause.
Not because something is wrong — but because the body is quietly adapting.
Many people notice these changes and move on.
"Probably nothing."
"I'm still active."
"I'll look into it later."
But here's what nearly 20 years of physical therapy experience has shown:
When these early signals aren't understood, movement often becomes more cautious — not weaker, just less automatic.
That's when confidence can start to feel inconsistent.
If this feels familiar, it's not because something is wrong — it's because balance is a skill most people are never shown how to practice intentionally.

Start Here: The Free Balance Awareness Discovery
A 5-minute discovery that brings clarity — not confusion.
- 6 awareness signals most people miss
- Personalized Balance Awareness Score
- Why exercise alone often isn't enough
- 3 simple observations to try this week
- Downloadable Starter Kit included
Balance Is a Brain Skill — Not a Leg Strength Issue
Most people are told that better balance comes from walking more, strengthening the legs, or staying active.
Those things help — but they don't explain why balance confidence changes.
Balance is created by how the brain and body communicate during movement.
The Brain-Balance Feedback Cycle™
Every time you stand, turn, or step forward — the brain processes signals from three systems:
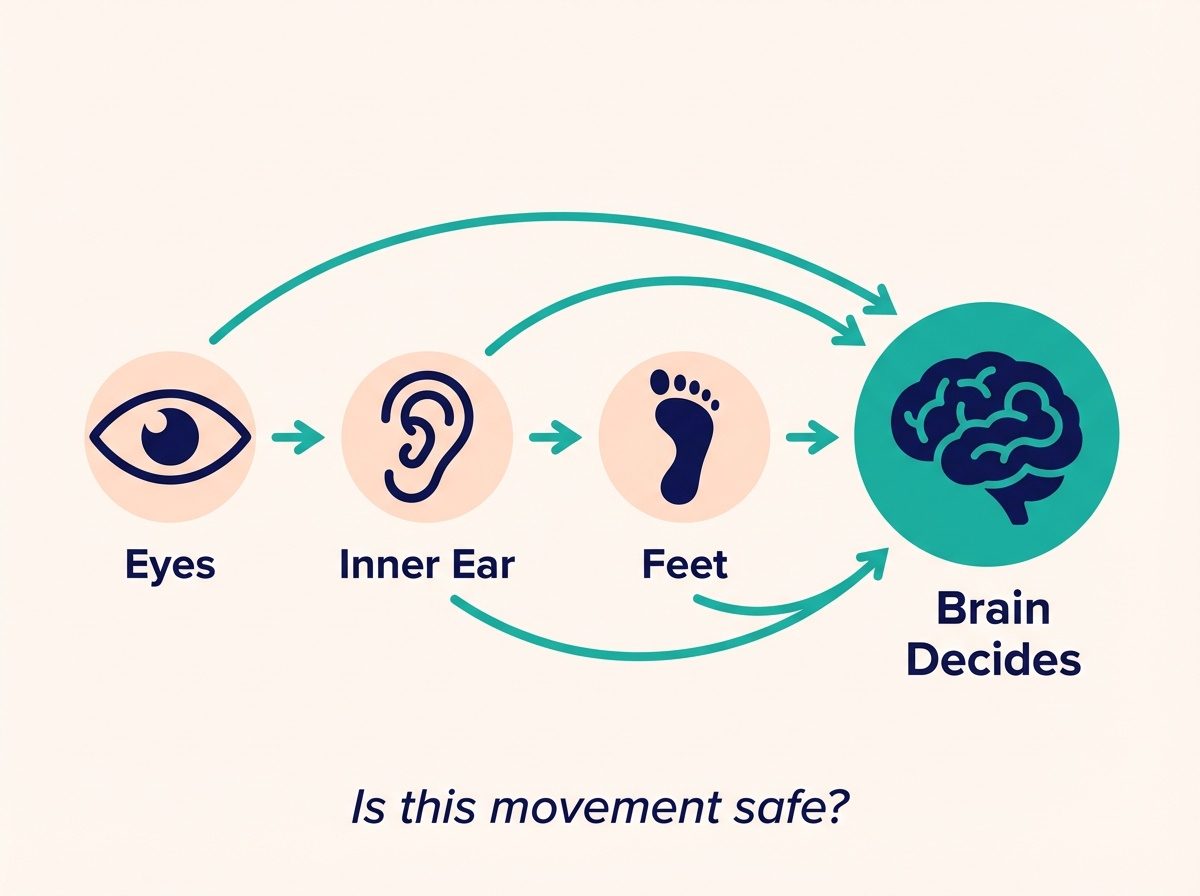
- → Eyes — What you see
- → Inner Ear — Where you are in space
- → Feet — What the ground feels like
When these signals work together smoothly, movement feels steady and automatic.
When they don't, movements start to feel less automatic — even when strength is still there.
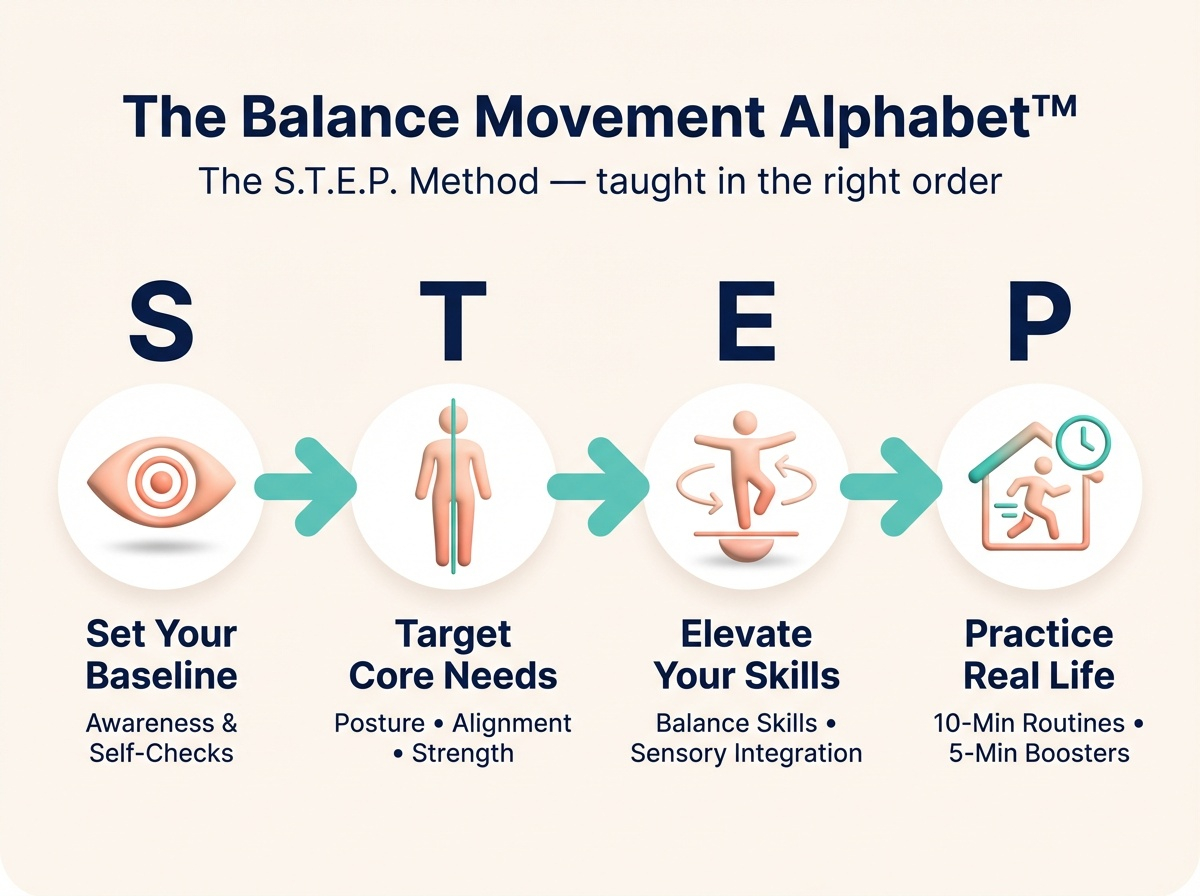
The Balance Movement Alphabet™
Instead of random exercises, the STEP into Balance System teaches balance in the order the brain understands:
-
S
Set Your Baseline Know where you're starting
-
T
Target Core Needs Address what matters most
-
E
Elevate Your Skills Build real-world steadiness
-
P
Practice Real Life Make it automatic
This is the difference between staying active — and training balance intentionally.
Ready to Build Real Balance Confidence?
The STEP into Balance System — A clear, step-by-step foundation designed by a Doctor of Physical Therapy.

STEP into Balance System
One-Time Payment — Lifetime Access
- → 5 Micro-Steps that build on each other
- → 3 Self-Checks to measure progress
- → 30+ Targeted Exercises (no gym, no equipment)
- → 10-Minute Guided Routines
- → 5-Minute Daily Boosters
- → Printable Guides & Progress Tracker
- → STEP into Practice Hub
- → 10-Day STEP into Confidence Email Series
Why I Created This System

After nearly two decades as a Physical Therapist, one question kept coming up:
"Why didn't anyone teach me this sooner?"
Many people I worked with were active, motivated, and doing what they thought they were supposed to do — walking, exercising, staying busy.
Yet they still felt hesitant with everyday movements like standing up, turning, or stepping down.
Not because they were weak.
But because no one had ever explained how balance actually works — or how to train it as a skill, not just exercise.
Most balance care is reactive. It waits until a problem feels urgent.
I wanted to create something different.
A clear, practical system that teaches the balance language the brain understands — early enough to make a real difference, and simple enough to use at home.
That's what became the STEP into Balance System.
Practice with purpose. Move with confidence. Live with independence.
Frequently Asked Questions
This system is designed for adults 55+ who want to improve balance at home. The exercises are gentle and progress gradually. However, if you have specific health concerns, consult your healthcare provider before starting any new movement practice.
No. Everything can be done at home using a sturdy chair and a wall or counter for support. No gym, no weights, no special equipment.
About 10 minutes a day. The routines are designed to fit into daily life — not replace it.
The system is simple to navigate. Videos play with one click. Printable guides are available if you prefer practicing without a screen.
The free Balance Awareness Starter Kit helps you understand where you're starting. The STEP into Balance System ($33) gives you the complete training — exercises, routines, and guidance to build real balance confidence.
Start Your Balance Journey Today
Whether you begin with the free Starter Kit or the full system, you're taking a step toward steadier, more confident movement.
Didn't Get Access?
You should receive access within 5 minutes of signing up.
If it's been longer, it's possible we have the wrong email — maybe a typo or missing info.
Please email us at:
Click to copy email address
Include: